
Īnother way glycated hemoglobin causes damage is via inflammation, which results in atherosclerotic plaque ( atheroma) formation. This leads to blood cell aggregation and increased blood viscosity, which results in impaired blood flow.
#Hemoglobin a1c normal range for female free#
Glycated hemoglobin causes an increase of highly reactive free radicals inside blood cells, altering the properties of their cell membranes. The use of hemoglobin A1c for monitoring the degree of control of glucose metabolism in diabetic patients was proposed in 1976 by Anthony Cerami, Ronald Koenig and coworkers. The reactions leading to its formation were characterized by Bunn and his coworkers in 1975.

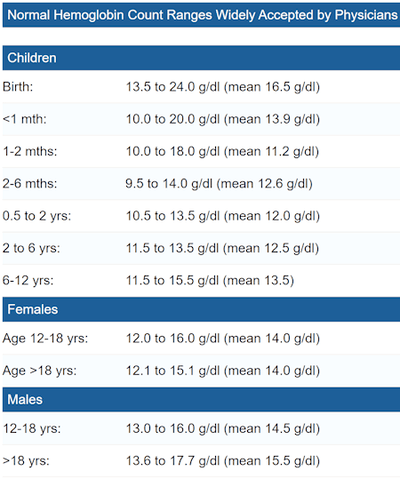
Its increase in diabetes was first described in 1969 by Samuel Rahbar et al. It was first characterized as a glycoprotein by Bookchin and Gallop in 1968. Hemoglobin A1c was first separated from other forms of hemoglobin by Huisman and Meyering in 1958 using a chromatographic column. Improved separation techniques have subsequently led to the isolation of more subfractions. The first fraction to separate, probably considered to be pure hemoglobin A, was designated HbA0, and the following fractions were designated HbA1a, HbA1b, and HbA1c, in their order of elution. The naming of HbA1c derives from hemoglobin type A being separated on cation exchange chromatography. The terms are still sometimes used interchangeably in English-language literature. Early literature often used glycosylated as it was unclear which process was involved until further research was performed. Glycated hemoglobin is preferred over glycosylated hemoglobin to reflect the correct (non-enzymatic) process. In diabetes, higher amounts of glycated hemoglobin, indicating poorer control of blood glucose levels, have been associated with cardiovascular disease, nephropathy, neuropathy, and retinopathy. As the average amount of plasma glucose increases, the fraction of glycated hemoglobin increases in a predictable way. Normal levels of glucose produce a normal amount of glycated hemoglobin. Since individual red blood cells have varying lifespans, the test is used as a limited measure of three months. The test is limited to a three-month average because the average lifespan of a red blood cell is four months. HbA1c is measured primarily to determine the three-month average blood sugar level and can be used as a diagnostic test for diabetes mellitus and as an assessment test for glycemic control in people with diabetes. The process by which sugars attach to hemoglobin is called glycation and the reference system is based on HbA1c, defined as beta-N-1-deoxy fructosyl haemoglobin as component. A1C is of particular interest because it is easy to detect. The formation of the sugar-hemoglobin linkage indicates the presence of excessive sugar in the bloodstream, often indicative of diabetes in high concentration (HbA1c >6.4%). However, glucose is less likely to do so than galactose and fructose (13% that of fructose and 21% that of galactose), which may explain why glucose is used as the primary metabolic fuel in humans. non-enzymatically) bond with hemoglobin when present in the bloodstream. Most monosaccharides, including glucose, galactose and fructose, spontaneously (i.e. Glycated hemoglobin ( HbA1c, glycohemoglobin, hemoglobin, A1C or A1c) is a form of hemoglobin (Hb) that is chemically linked to a sugar.

Form of hemoglobin chemically linked to a sugar Glycated hemoglobin


 0 kommentar(er)
0 kommentar(er)
